Is Osteoporosis a Barrier to Dental Implants?

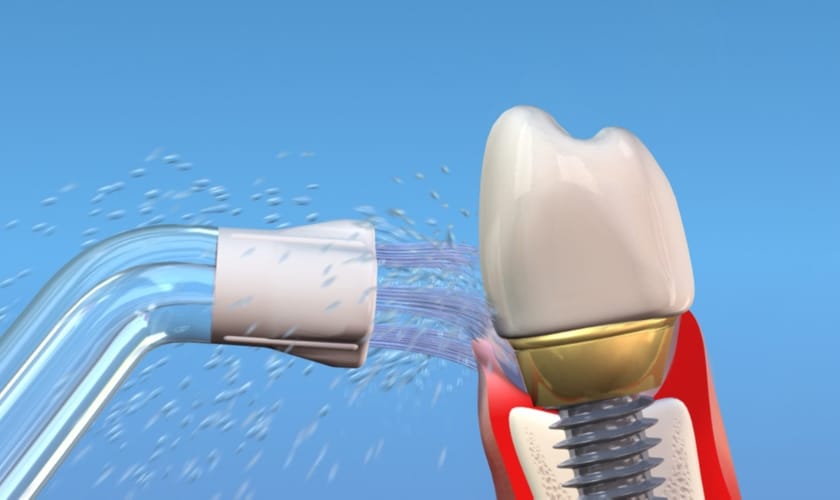
Osteoporosis, a condition that weakens bones, often raises concerns about dental health. Many people wonder if osteoporosis poses a barrier to getting dental implants. Dental implants offer a permanent solution for missing teeth, improving both function and appearance.
However, the success of implants depends on the strength and density of the jawbone. This dependency raises important questions for those with osteoporosis.
In this blog, we explore the relationship between osteoporosis and dental implants. We will examine how osteoporosis affects bone health, especially in the jaw, and what it means for dental implant candidates.
We will also discuss the criteria for dental implant candidacy, potential challenges, and the precautions necessary for a successful procedure. Whether you have osteoporosis or care for someone who does, understanding these factors will help you make informed decisions about dental implants.
Let’s dive into the facts and find out if osteoporosis truly stands in the way of achieving a healthy, beautiful smile.
Understanding Osteoporosis
Osteoporosis is a medical condition where bones become weak and brittle. It occurs when the creation of new bone doesn’t keep up with the removal of old bone. This imbalance leads to porous and fragile bones, increasing the risk of fractures.
Causes:
- Aging: Bone density decreases naturally with age.
- Hormonal changes: Menopause in women and low testosterone in men.
- Nutritional deficiencies: Lack of calcium and vitamin D.
- Lifestyle factors: Sedentary lifestyle, smoking, and excessive alcohol use.
How It Affects Bone Density and Strength?
Osteoporosis reduces bone density and strength, making bones more susceptible to fractures. In the jaw, this condition can compromise the bone structure needed for dental implants.
- Bone Density: Lower density means less support for implants.
- Bone Strength: Weaker bones can fail to integrate with implants, risking implant stability.
- Overall Health Impact: Osteoporosis affects the entire skeletal system, including the jaw, impacting oral health and implant success.
Connection Between Osteoporosis and Oral Health
Osteoporosis, a condition characterized by weakened bones, significantly impacts oral health, particularly the jawbone and overall dental health.
Impact on Jawbone
- Bone Density Reduction: Osteoporosis leads to decreased bone density in the jawbone, affecting its ability to support teeth and dental implants.
- Increased Risk of Tooth Loss: Weakened jawbone structure makes teeth more prone to looseness and eventual loss.
- Compromised Healing: Bone healing processes are slower and less effective in osteoporotic jaws, affecting recovery from dental procedures.
Effects on Overall Dental Health
- Periodontal Disease: Osteoporosis increases susceptibility to gum disease due to weakened bone support around teeth.
- Dental Implant Complications: Implant success rates may decrease as the weakened jawbone may not integrate well with the implant.
- Prosthetic Challenges: Difficulty in fitting dentures or other dental prosthetics due to changes in jawbone structure.
- Bone Resorption: Osteoporosis accelerates bone resorption, where bone is broken down faster than it is replaced, further compromising oral health.
Criteria for Dental Implant Candidacy
Ensuring candidacy for dental implants involves meeting general requirements, which are particularly nuanced for patients with osteoporosis.
General Requirements
- Sufficient Bone Density: Adequate jawbone volume and density to support the implant.
- Healthy Gums: Absence of active gum disease to ensure successful integration.
- Overall Health: Good general health to undergo surgery and heal effectively.
Considerations for Patients with Osteoporosis
- Bone Density Assessment: Detailed evaluation of jawbone density using imaging techniques.
- Treatment Plan Adjustments: Potential adjustments in treatment planning to accommodate bone health.
- Consultation with Specialists: Collaboration with osteoporosis specialists to optimize bone health before implant placement.
Challenges of Dental Implants with Osteoporosis
Implanting dental fixtures in patients with osteoporosis presents unique challenges and considerations due to bone health complexities.
Risks and Potential Complications
- Bone Integration Issues: Reduced bone density can hinder proper osseointegration of implants.
- Increased Fracture Risk: Higher susceptibility to bone fractures during or after implant surgery.
- Healing Challenges: Slower healing process and potential for delayed bone fusion around implants.
Studies and Research Findings
- Success Rates: Varied success rates reported in studies, influenced by patient-specific factors and treatment protocols.
- Long-term Outcomes: Research indicates mixed long-term outcomes, emphasizing the need for tailored treatment plans and close monitoring.
Preparation and Precautions for Dental Implants
Before undergoing dental implant surgery, several crucial preparations and precautions are necessary to ensure optimal outcomes, especially for patients with osteoporosis.
Pre-Implant Treatments and Evaluations
- Periodontal Assessment: Comprehensive evaluation of gum health to address any existing periodontal disease.
- Medical Evaluation: Thorough review of medical history to identify underlying conditions such as osteoporosis and their implications.
- Bone Density Scans: Essential imaging to assess bone quality and quantity, crucial for determining implant candidacy and planning.
Importance of Bone Density Scans and Medical History
- Risk Assessment: Identifying risks associated with osteoporosis and potential complications during and after surgery.
- Treatment Planning: Tailoring implant placement and type based on bone density results and medical history insights.
- Enhanced Predictability: Improving the predictability of implant success through detailed pre-operative assessments.
Treatment Options and Alternatives
For patients with severe osteoporosis, various treatment options and alternatives to traditional dental implants are available to address specific challenges and ensure successful oral rehabilitation.
Bone Grafting and Supportive Procedures
- Bone Augmentation: Enhancing bone volume and density through grafting techniques to provide adequate support for implant placement.
- Sinus Lift: Elevating the sinus floor to create space for bone grafts and promote stable implant anchorage in the upper jaw.
- Ridge Expansion: Widening the jawbone ridge to accommodate implants and improve stability.
Alternatives to Dental Implants
- Fixed Dental Bridges: Traditional bridges supported by adjacent teeth, suitable for patients with compromised bone density.
- Removable Dentures: Complete or partial dentures that can be easily removed and cleaned, offering flexibility and function.
- Implant-Supported Dentures: Combining implants with dentures for enhanced stability and retention, even in cases of reduced bone density.
Understanding how osteoporosis impacts dental implant candidacy is crucial for informed decision-making. Despite challenges, advancements in dental technology and treatment options offer viable solutions. Consulting with a qualified dental professional ensures personalized care and optimal outcomes.